Article
Key Performance Indicators in Irish Hospital Libraries: Developing
Outcome-Based Metrics to Support Advocacy and Service Delivery
Michelle Dalton
Librarian, HSE Mid-West Library & Information
Services
University of Limerick
Limerick, Ireland
Email: michelledalton@gmail.com
Received: 6 June 2012 Accepted:
10 Sept. 2012
 2012 Dalton.
This is an Open Access article distributed under the terms of the Creative
Commons‐Attribution‐Noncommercial‐Share Alike
License 2.5 Canada (http://creativecommons.org/licenses/by-nc-sa/2.5/ca/),
which permits unrestricted use, distribution, and reproduction in any medium,
provided the original work is properly attributed, not used for commercial
purposes, and, if transformed, the resulting work is redistributed under the
same or similar license to this one.
2012 Dalton.
This is an Open Access article distributed under the terms of the Creative
Commons‐Attribution‐Noncommercial‐Share Alike
License 2.5 Canada (http://creativecommons.org/licenses/by-nc-sa/2.5/ca/),
which permits unrestricted use, distribution, and reproduction in any medium,
provided the original work is properly attributed, not used for commercial
purposes, and, if transformed, the resulting work is redistributed under the
same or similar license to this one.
Abstract
Objective – To
develop a set of generic outcome-based performance measures for Irish hospital
libraries.
Methods
– Various models and
frameworks of performance measurement were used as a theoretical paradigm to
link the
impact of library services directly with
measurable healthcare objectives and outcomes. Strategic objectives were
identified, mapped to performance indicators, and finally translated into
response choices to a single-question online survey for distribution via email.
Results
– The set of performance indicators
represents an impact assessment tool which is easy to administer across a
variety of healthcare settings. In using a model directly aligned with the
mission and goals of the organization, and linked to core activities and
operations in an accountable way, the indicators can
also be used as a channel through which to implement action, change, and
improvement.
Conclusion
– The indicators can be adopted at a
local and potentially a national level, as both a tool for advocacy and to
assess and improve service delivery at a macro level. To overcome the
constraints posed by necessary simplifications, substantial further research is
needed by hospital libraries to develop more sophisticated and meaningful
measures of impact to further aid decision making at a micro level.
Introduction
Quantitative measures of performance are an essential
management tool in any organization. Key performance indicators (KPIs) help
them meet key strategic objectives, drive and deliver change, and assess the
impact and effectiveness of services. Appropriate metrics not only provide a
high-level snapshot of service levels at any given point in time, but also help
to inform the operational activities and tasks that contribute to achieving the
key strategic goals of the organization.
Within the health science library sector in Ireland,
the primary performance measures are typically input-based metrics, usage
statistics, and other operational measures (Harrison, Creaser, & Greenwood,
2011). These statistics typically include gate counts, borrowing totals, the
number of books held per staff member, the cost per use of electronic
resources, the number of reference queries answered, or the number of
information literacy sessions delivered. As largely input- or usage-focused
indicators, these measures capture activity levels effectively but represent
extremely blunt tools for assessing real effectiveness and impact. In contrast,
outcome measures capture the “impact or effects of library services on a
specific individual and ultimately on the library’s community” (Matthews, 2008,
p. xiv). This very evidence is becoming increasingly important in order to
promote, and advocate for, the value of health science libraries, and in
particular hospital libraries – or as Ritchie (2010, p. 1) succinctly advises:
“knowing why you exist (not simply what you do).”
In this respect hospital libraries have a unique
raison d’être. They are required to support a number of mission critical goals
within the institution from “saving hospitals thousands of dollars per year to
saving patients’ lives” (Holst et al., 2009, p. 290). The value chain within
which hospital libraries must position themselves requires:
Providing the right information at the right time to enhance medical
staff effectiveness, optimize patient care, and improve patient outcomes … save
clinicians time, thereby saving institutions money… provide an excellent return
on investment for the hospital, playing a vital role on the health care team
from a patient’s diagnosis to recovery. (Holst et al., 2009, p. 290)
However, given the absence of any robust quantitative
evidence regarding the value contributed by hospital libraries in Ireland, such
claims remain largely unsubstantiated, and may even appear merely aspirational
to some.
The use of performance indicators is now commonplace
across nearly all aspects of the Irish healthcare sector, including public
health services which are administered by the Health Service Executive (HSE).
In recognition of the need for an effective assessment tool, the HSE designed
and implemented the HealthStat system. The indicators
incorporated in HealthStat provide an overview of how
services are delivered using a broad range of various performance measures.
Notably, however, there are currently no library-related service indicators
included within the system, or indeed within any of the systematic or
standardized assessment frameworks which are implemented by the HSE (Health
Service Executive, 2011). Indeed, the Report
on the Status of Health Librarianship & Libraries in Ireland (SHeLLI ) articulated the pressing need for health science
libraries in Ireland to establish “a body of evidence, with performance
indicators, available at the level of individual
libraries and nationally, used
for service promotion and advocacy” (emphasis added) (Harrison et al., 2011, p.
42). In this context, the aim of this study was to develop a potential set of
performance measures sufficiently general to be applied to other libraries in
broadly similar settings nationally, whilst still retaining some value at a
local level (in this case, a library based within an acute hospital).
Literature
Review
An Outcome Based Approach to Measurement
Effective performance measurement intrinsically
requires measuring the “right” things in the “right” way. It is a complex task,
however, to distill a library’s core activities,
functions, and goals into a narrowly defined, yet sufficiently powerful, set of
indicators.
KPIs can be viewed through a variety of lenses,
including:
- the goal attainment model driven by strategic
objectives
- the systems resource model of input measures
- the internal systems model derived from workflows
and communications processes
- the multiple constituencies model based on the
extent to which different stakeholders’ needs are met
(Cameron,
1986)
In the context of impact assessment, the goal
attainment model offers a particularly good fit. Within this framework, the
inputs (e.g., operational activities and decisions) that drive performance
indicators should also impact on the organization’s strategic objectives and
desired outcomes (Hauser & Katz, 1998). For instance, a desired objective
of a hospital may be to deliver efficient and timely patient care, and a
relevant performance indicator for the library could be to save clinicians’
time as a result of using library services. Corresponding inputs may include
reconfiguring or streamlining workflows and staffing arrangements in order to
reduce the response times for clinical information queries. These same inputs
should also impact on the overarching objective of efficient patient care,
which in this case is a reasonably logical hypothesis, a priori. These
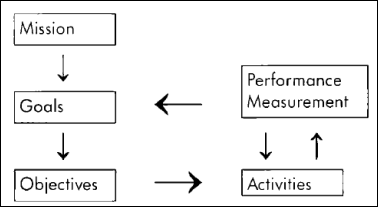
relationships and interdependencies also mirror Boekhorst’s
(1995) model of performance measurement, which emphasises the direct links
between goals and objectives, and performance measurement and activities, allowing
operational tasks to be consistently aligned with strategic aims.
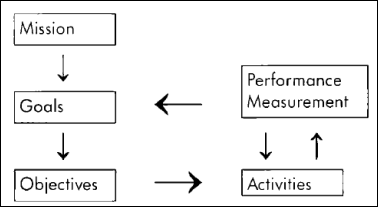
Figure
1
Boekhorst’s
model of performance measurement (Md Ishak & Sahak, 2011, p.5)
Matthews’s (2008) balanced scorecard model adapted
from Kaplan and Norton (1992) also adopts a strategic focus with respect to
measurement. Performance indicators should reflect the organization’s strategy
across four perspectives: financial, customer, internal business processes, and
learning and growth. Outcome measures that help to assess key strategic
objectives can play an important role as part of this approach. Matthews breaks
the concept of outcomes into immediate, intermediate, and ultimate outcomes,
shifting in focus from creating value at the individual level to the overall
impact on the organization. Effectively measuring these outcomes can help the
organization to communicate its long-term or strategic value to users.
Donabedian’s (1966) seminal work on evaluating medical
care frames the concept of quality assessment within a model of structures,
processes, and outcomes – in other words, the resources used by the
organization, the activities carried out in healthcare delivery, and the
outcomes on patient care. Appropriate performance indicators can be used within
the framework to capture and measure key elements in this chain, therefore
helping to assess the overall quality and performance of the healthcare system.
However, libraries are perhaps guilty of an
overreliance on a structural approach in this regard, by focusing on measuring
the inputs and resources used to deliver desired outcomes, in spite of “the
major limitation that the relationship between structure and process or
structure and outcomes, is often not well established” (p. 695). This argument
reinforces the need for objective outcome-based indicators in order to assess
the performance of hospital libraries in a valid and meaningful way.
“Ultimately, the goal of health care is better health,
but there are many intermediate measures of both process and outcome” (WHO,
2003, p. 5). Holst et al. (2009) identify three core channels through which
hospital libraries can potentially add real value: patient outcomes, time
savings, and cost savings. These variables are not exogenously determined, and
indeed saving the time of clinical staff will also,
all other things being equal, reduce costs and improve patient outcomes as
staff can treat more patients in the same amount of time. By focusing on these
three channels, this study is limited to an attempt to capture and assess the
value of library and information services to clinical practice and outcomes,
rather than the contribution which hospital libraries also make to research
output. The latter is obviously another channel through which hospital
libraries add value, but constructing a suitable indicator to measure this
variable is outside the scope of this study. This also largely reflects the core mission of the HSE in its
focus on patient care (Health Act, 2004).
Developing Well-Designed and Actionable Indicators
Loeb contends that “the central issue in performance
measurement remains the absence of agreement with respect to what should be
measured” (2004, p. i7). The Health Information and Quality Authority of
Ireland (HIQA) recommends that performance indicators
used to measure healthcare quality should exhibit certain properties:
- Provide a comprehensive view of the service
without placing an undue or excessive burden on organizations to collect
data.
- Be explicitly defined and based on high-quality
and accurate data.
- Measure outcomes which are relevant and
attributable to the performance of the healthcare system in which they are
employed.
- Not be selected based solely on the availability
of data.
- Be supported by local measures in order to inform
practice and operations at a local level.
(HIQA, 2010, p. 20-1)
These principles provide a baseline standard for
performance measures in this study. Parmenter (2010)
extends these properties further, outlining the typical attributes of effective KPIs as measures that are
non-financial, frequently measured, acted on by senior management, indicating
the necessary action required by staff, tying responsibility down to a team or
individual, having a significant impact, and encouraging appropriate action.
Here the emphasis on action is notable. Frequently data may be collected as a
matter of routine or obligation but not effectively utilized or acted upon.
However, in contrast with usage statistics or input-based metrics, outcome-based
indicators are, by definition, directly driven by core strategic objectives,
and therefore are inextricably linked with the actions supporting these goals.
Consequently, outcome-derived KPIs can be channelled more easily into concrete,
actionable insights, resulting in real changes in systems, processes, and
services.
Supporting Good Governance through Assessment and
Accountability
Quantitative performance indicators also have a role
to play in providing an objective assessment of services and in both internal
and external consistency in the decision-making process. External reporting,
transparency, and compliance are critical dimensions of good governance. The
organizational structure of hospital libraries is also changing (Harrison et
al., 2011). Staffing pressures dictate that an increasing number of healthcare
libraries in Ireland are likely to be run by solo librarians in the future,
with a single individual having responsibility for managing all aspects of library
services. This further increases the need for external and objective measures
to serve as a verifiable cross-check on services.
Appropriate outcome-based KPIs stimulate action in a
way which also attributes responsibility. As it must be made clear who “owns”
each indicator, this increases accountability within the organization.
Achieving this buy-in successfully in practice requires building an environment
centred on trust, whereby performance measures and targets are clearly
communicated, understood, and accepted as fair by all staff and stakeholders.
However, if KPIs are derived directly from strategic objectives and outcomes,
it is often easier for the individuals concerned to see the relevance of and
need for such measures, and staff are therefore more
likely to view assessment in a positive way.
Evidence Based Advocacy
A significant body of literature already exists on the
importance of impact assessment as a tool for advocacy in hospital libraries
outside Ireland. Weightman and Williamson’s systematic
review of library impact (2005) appraises 28 studies which each assess at least
one direct clinical outcome. Survey instruments are the most frequently used
method of data collection, but in most cases the limitation of “desirability
bias” (p. 6) arising from self-selection is highlighted as a weakness. Twenty
different impact measures are recorded from the studies based in the
traditional library setting, indicating that some level of variation exists as
to which outcomes are perceived as the most critical in influencing patient
care.
The landmark Rochester Study (Marshall, 1992) is
included in Weightman and Williamson’s (1995) review.
The historical context, marked by a change to U.S. federal requirements
regarding hospital library provision in 1986, sparked the need for potent
advocacy tools to improve the “visibility and status of the library” by
expressing value in “the bottom line,” that is, the impact on clinical decision
making (p. 170). The study adopted a relatively detailed approach in measuring
the impact of library use specifically on physicians’ practice, including
aspects such as the choice of tests, drug treatment, and patient advice. As it
is hoped that the indicators generated by this research can be used to
demonstrate the value of services to a broader range of health and social care
professionals (including management and administrative staff) reflecting a
multidisciplinary approach to healthcare, this level of detail was rejected in
favour of higher level indicators to avoid causing confusion by
presenting respondents with irrelevant or excessive choices. Moreover, as the SHeLLI report (2010) indicates, there is a need for a
national measure, and as significant heterogeneity exists across regions and
local healthcare facilities across Ireland, some simplification is unavoidable.
Further qualitative research, such as structured interviews which could be
tailored to a specific discipline or local context, could help to pinpoint and
elucidate concrete or specific examples of impact, but this falls outside the
scope of the present study.
In some healthcare institutions there has been an
increased shift towards outsourcing, redeployment, and the use of “shared
services” models in recent years, precipitated by the economic and political landscape
(Harrison et al., 2011). Libraries have not been immune to such developments,
and indeed have even been seen by some as easy targets in the potential for
cost savings (Geier, 2007). However, Ritchie contends
that in many cases such decisions are in fact based on clear economic arguments
that stand up to valid and rigorous cost-effectiveness analysis. These evidence
based financial rationales pose “very real threats to our survival, and serious
challenges to our ability to develop and thrive; and we have to be able to
justify our existence in their terms” (2001, p. 1). But the SHeLLI
report notes that “there is currently little, if any, evidence of the impact of
health information services – how the use of library services and/or resources
feeds into direct patient outcomes or financial benefits” (Harrison et al.,
2011, p. 7).
It is unclear why there is a lack of such measures
within the Irish hospital library environment. It can perhaps be in partly
attributed to the lack of data and integrated evidence base within the
healthcare sector generally. Indeed Levis, Brady, and Helfert
(2008) draw attention to this problem, noting that:
Computerised information systems have not as yet achieved the same level
of penetration in healthcare as in manufacturing and retail industries. In
Ireland many serious errors and adverse incidences occur in our healthcare
system as a result of poor quality information. (p. 1)
However, initiating a culture of accountability and
outcome-based performance assessment can and should be a positive development
for libraries, and one which provides a rare and valuable opportunity to
leverage evidence based advocacy. Librarians as a profession may understand the
benefits that effective information services can offer to an organization, but
this is not enough. Hospital libraries must articulate and verifiably
demonstrate the value of their services in the language which is understood by
the commercial and corporate world: that is, by expressing their services as
strategic objectives, outcomes, and value for money.
Methods
The study is underpinned by a broadly
positivist approach, and various models and frameworks are used as a
theoretical paradigm to inform the development of a potential set of
quantitative performance indicators. As the
aim of this research specifically relates to the impact assessment of library
services on measurable healthcare outcomes and objectives, Cameron’s (1986)
goal attainment model was selected as the most appropriate framework within
which to place the analysis. Boekhorst’s (1995) model
of performance measurement was used as a lens through which to identify and analyze the relationships and links between the HSE’s
mission and strategic objectives, and library performance and activities. This
reflected the need to look beyond the mission and
goals of the library itself towards those of the parent organization.
For the purpose of this study, the model was simplified slightly by combining
the goals and objectives into a single element.
In order to construct outcome-based indicators, a
clear picture was needed of the organization’s mission,
and the strategic objectives and desired outcomes of the acute hospital sector
in Ireland.
Organizational Mission
The HSE was established under the Health
Act 2004 as the single body with statutory responsibility for the management
and delivery of health and personal social services in the Republic of Ireland.
As outlined in the act, “the objective of the Executive is to use the resources available to it in the
most beneficial, effective and efficient manner to improve, promote and protect
the health and welfare of the public” (2004, pt. 2, s.7). This statement was selected as the
overall organizational mission for the model.
Strategic Objectives and Outcomes
Given the aim of developing a set of
performance indicators which are sufficiently broad to be applied across
multiple hospital settings, the key strategic objectives were identified from
the Report of the National Acute Medicine
Programme (2010), a framework document for the delivery of acute medical
services to improve patient care. The report highlights eight overarching aims
of the programme as follows:
1. Safe, quality care.
2. Expedited diagnosis.
3. The correct treatment.
4. An appropriate environment.
5. Respect of their [patients’] autonomy and
privacy.
6. Timely care from a senior medical doctor
working within a dedicated-multidisciplinary team.
7. Improved communication.
8. A better patient experience.
(Health Service Executive & Royal College of
Surgeons Ireland, 2010, p. 1)
These objectives clearly do not operate
exogenously, and there is likely to be some correlation between them.
Therefore, in view of the need to develop a set of pragmatic, measurable and
high-level indicators, these eight individual objectives were assessed and grouped together based on commonality. From this
process, three primary objectives emerged: quality of patient care, safety of
patient care, and efficiency/speed of patient care.
These objectives are also congruent with
Holst et al.’s (2009) analysis of the channels through which hospital libraries
can deliver value: improved patient outcomes, saving clinician’s time, and
reducing costs. Furthermore, they also directly mirror three of the five core
domains of healthcare quality which are identified by HIQA (2010). The two
remaining dimensions, equality of care and person-centredness,
were not included, as library services were viewed to have limited, if any,
influence over these aspects.
Key Performance Indicators
The final stage required mapping these conceptual
objectives into a set of explicit indicators. As well as being directly linked
to the organizational mission and objectives, it was critical that the
indicators should also be consistent with the recommendations outlined in
HIQA’s Guidance on Developing Key
Performance Indicators and Minimum Data Sets to Monitor Healthcare Quality
(2010).
A comprehensive literature review was undertaken to
identify the primary operational factors that influence the quality, safety,
and efficiency/cost of healthcare, which library services can also support.
However, these three concepts are broad and complex variables that can be
measured and assessed through myriad different indicators. Even 50 years on,
Klein’s (1961, p. 144) conclusion that “there will never be a single
comprehensive criterion by which to measure the quality of patient care” still
holds some degree of weight. For this reason, broad indicators relating to
improvement in patient care or practice were chosen as proxies, rather than
drilling down into more specific diagnostic or therapeutic outcomes –
reflective of Donabedian’s general “yardstick” of
specificity rather than a “watertight, logic-system” (1966, p. 703). Whilst
this may represent a somewhat vague and normative standard open to an element
of ambiguity as to what constitutes improvement or reduction, it was viewed as
a necessary compromise, given the need to apply the indicators across disparate
health and social care contexts to reflect a multidisciplinary approach, and
indeed varying hospital environments.
Data Collection and Administration of Survey
A survey questionnaire was selected as the data
collection instrument to measure the indicators due to the simplicity and cost
of administration. One of the key aims of the questionnaire design process was
to ensure that the burden on respondents was minimized. This is particularly
germane to the healthcare setting, as doctors typically exhibit a low to
moderate response rate to survey questionnaires (Olmsted, Murphy, McFarlane,
& Hill, 2005). Indeed, poor response rates to previous surveys required an
innovative approach as to how the instrument could be packaged effectively to
busy clinical and management staff to best encourage response. For this reason,
the survey was deliberately branded as “one question” rather than as a survey,
to highlight the simplicity and minimal time commitment involved on the part of
the respondent.
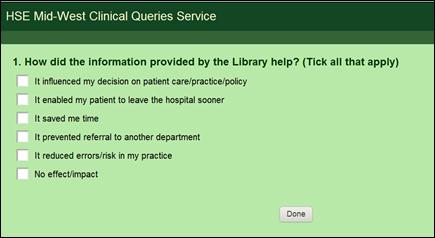
To produce the final survey, the five performance
indicators were incorporated as possible responses to the question: “How did
the information provided by the Library help?” Hospital staff are also free to indicate
that the information provided had no impact or effect. In phrasing both the question and responses, the Plain Language Style Guide for Documents
(HSE & NALA, 2009) was consulted to ensure clarity of expression. The
survey was also piloted with a number of clinical and library staff to ensure
that it was easy to interpret and understand.
The online survey tool SurveyMonkey
was used to administer the question, and a survey link was included with the
responses to any clinical information or reference queries of substance. It is
difficult to classify “substance” in an objective way across all local
contexts, however it is generally assumed to refer to strategy- or consultation-based
queries, as clarified by Warner (2001). In practice, this refers to complex
mediated literature searches, where a full search report and supporting
documentation are returned to the user. Such queries are received from
healthcare (physicians, nurses, and allied health professionals) and health
management staff, and thus the potential survey population is relatively
disparate. This in turn necessitates the need for the survey responses to be phrased
using terminology sufficiently general to be applicable across a range of
hospital contexts. As the link is included in response to a specific,
individual query or transaction, it is clear to the user that the survey
relates explicitly to this particular interaction rather than to library or
information services in a more general sense. No explicit incentive is offered
to encourage completion of the survey, but as it is included within
personalized correspondence and search results, rather than as a generic
promotional email, this may in itself prompt users to respond after they have
assessed the information. All responses received are anonymous and subjects are
made aware of this. The survey instrument has been designed to be replicated in
other similar hospital libraries, so that data can be pooled in order to
generate significant sample sizes for future analysis and interpretation. We
plan to analyze and report survey results every six
months, with the provision that sample sizes are sufficient to generate
meaningful insight.
Results
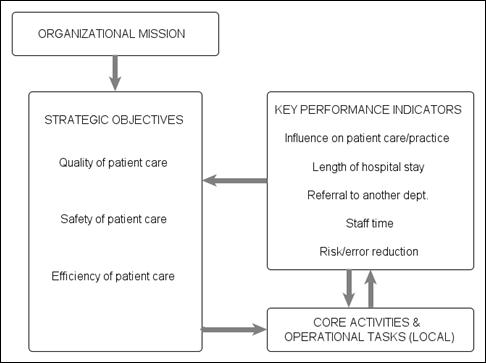
Informed by the organizational mission and three core
strategic objectives listed above, the final performance indicators selected
were:
- Influence on patient care or guiding of clinical
practice/policy.
- Length of hospital stay.
- Referral to another department.
- Staff time.
- Risk/error reduction.
At the local level, these indicators can subsequently
be mapped to a corresponding set of core library activities and tasks that
influence each measure, that is, library-specific inputs such as staff
workflows, resources, and local systems to help support decision making.
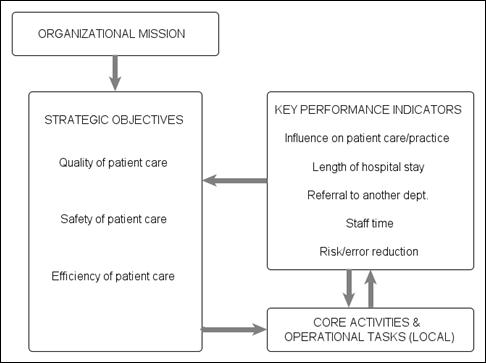
Figure 2
Flowchart
of strategic objectives and indicators (Adapted from Boekhorst,
1995)
When
translated into survey responses, these indicators were presented to staff
through the SurveyMonkey interface as illustrated in
Figure 3.
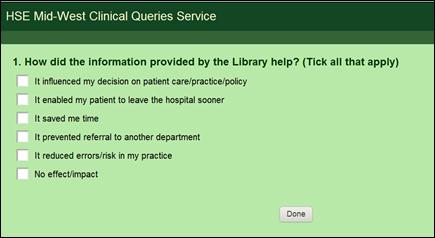
Figure
3
Presentation
of online survey question to users
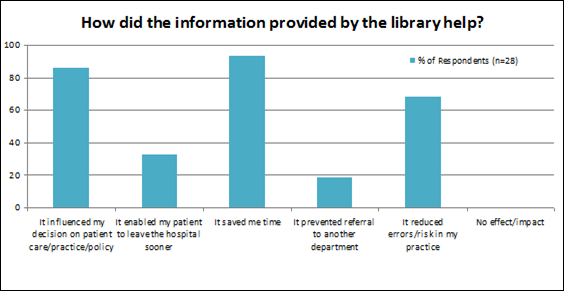
Results from the responses received during the six-month
period since the survey was initially introduced are illustrated below. A total
of 93% of staff stated that the information provided by the library had saved
them time, and 86% claimed it had influenced their decision on patient care,
clinical practice, or policy – a broadly similar proportion to that estimated
in the Rochester Study with significantly larger sample sizes (Marshall, 1992).
With over half of respondents indicating that risk or errors had also been
reduced, these results suggest at least some positive impact of library
services on key strategic objectives. No respondents indicated that the
information failed to have any effect or impact; however it is likely that this
is in part due to self-selection bias from the nature of the survey – a common
limitation, as highlighted by Weightman and
Williamson (2005). Further research would be needed to estimate the extent to
which this factor influences the overall results. As a tool for advocacy, a
single snapshot of data offers some value, but as performance indicators,
survey results are only really meaningful when compared over time or in a
cross-sectional context, and so these initial results are of limited value in
assessing library services in relative terms. To date the survey has been
rolled out in only one regional area. Thus, while of value at a local level,
the real potential for a national-level indicator remains untapped.
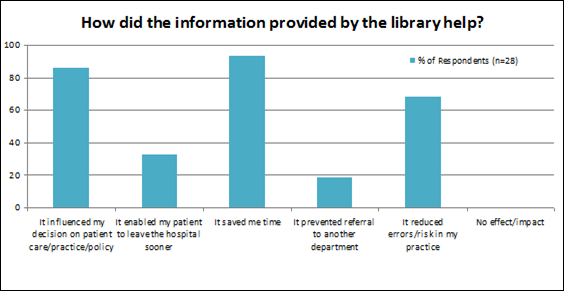
Figure
4
Responses
received from online survey
Discussion
Application as a Tool in Practice
The need for objective and quantitative performance
measures in hospital library settings is clear (Harrison et al., 2011; Ritchie,
2010). Outcome-based measures that reflect critical outputs and outcomes are
invariably more visible than demand-derived metrics, which offer little or
nothing from a marketing and advocacy point of view (Chan & Chan,
2004). If an instrument such as this
survey could be applied in a standardized way to produce a national measure of
performance, benefits would likely accrue, not only in fostering a culture of
objective and continuous assessment to drive local service improvements, but
also as a valuable tool for evidence based advocacy. Furthermore, extending the
survey more widely would also offer the potential to obtain larger sample sizes
for increased reliability, precision, and statistical power. More sophisticated
analysis may also be possible. Data could be used to identify any statistically
significant differences across hospitals or regions. In addition, results could
be used to estimate the correlation, if any, between the outcomes achieved and
levels of inputs (for example, library budgets or staff numbers) either on a
cross-sectional or time series basis.
Notwithstanding these advantages, there is no
guarantee that using these performance indicators will deliver a real change in
hospital or clinical practice. Improvement requires more than tracking and
monitoring data and identifying problems. It must be accompanied by real
action, buy-in, and commitment from stakeholders in a visible and accountable
way. In essence, “providing managers and staff with accurate, intuitive, and
easily interpretable data is one third of the recipe for improvement. The other ingredients are alignment with strategic objectives and a
system for accountability” (Wadsworth, 2009, p. 69). In view of this, it
is hoped that by developing the indicators using a model directly aligned with
the strategic mission and goals of the organization and linked to core
activities and operations in an accountable way, the
performance measures documented above will also facilitate real and meaningful
follow-through on change.
Limitations
The questionnaire developed for this article
represents a substantial simplification in assessing the efficiency and quality
of patient care, and intrinsically represents a self-assessment by the user.
Firstly, positive self-selection (or desirability bias as discussed in Weightman & Williamson (1995)), whereby those who find
the service of greater value are more motivated to respond to the survey question,
may introduce bias into the results. Indeed it is a more-than-plausible
hypothesis that those who do not value the library’s services will simply not
respond to the questionnaire. It is likely that this is in part responsible for
the fact that no respondents indicated that the information provided to them
had no effect or impact. As the survey is directly linked to a specific
transaction, it also excludes non-users by definition – a further limitation.
Moreover, whilst staff may claim that the research and information support
provided by the library saved them time or reduced the risk of errors in their
practice, this assessment may be subject to bias or variance in interpretation
among the respondents. There is something of a Catch-22 at play in this
respect. The need for widely applicable indicators for the reasons outlined
above necessitates a significant degree of generality in specification.
However, this same generality leads to an increased dependence on “the
interpretations and norms of the person entrusted with the actual assessment” (Donabedian, 1966, p. 704). Striking the right balance
between both needs is a challenge.
The value of the results generated by the survey could
be significantly enriched by additional qualitative data obtained through
interviews or focus groups. A mixed methods approach such as this would help to
capture the story behind the quantitative headlines, and also yield greater
insight into why, when, and how hospital staff use the library. As survey
responses are anonymous, a separate recruitment process would have to be
undertaken to identify potential interviewees, and to include non-users also to
help address the aforementioned limitations.
Conclusion
In spite of the limitations outlined above, the
absence of any real outcome-based measure within the Irish hospital library
sector is simply too pervasive to ignore. Whilst the indicators and data
collection framework proposed in this study may be formative and incipient at
best, there is a clear need for evidence of impact to help fill the gap which
exists at present between library services and hospital outputs, outcomes, and
objectives. Perhaps it is time for Irish hospital librarians to redirect some
of their time and effort away from collecting solely input and usage focused metrics, and towards
developing meaningful outcome-based measures? Given that efficacy is such a key
driver in healthcare, the former are of limited insight, whilst “the validity
of outcome as a dimension of quality is seldom questioned” (Donabedian,
1966, p. 693). Instead of focusing on measuring activities and inputs in
isolation as libraries have often done in the past, adopting an outcome-based
model allows key objectives and the need for accountability to drive service
delivery, ultimately ensuring that library services remain relevant to,
consistent with, and of direct value to the organization. Traditional measures
of activity can still tell a valuable story, but an alternative narrative is
also required.
Given the aim of creating broadly generic indicators
which are measureable in practice and transferable across a variety of contexts
(internal and external), simplification is a pragmatic and necessary
constraint, but as Tukey argues: “Far better an approximate
answer to the right question, which is often vague, than an exact answer to the
wrong question, which can always be made precise” (1962, p. 13). It is hoped, therefore, that this initial framework
can provide a platform for Irish hospital libraries to assess performance at a
macro level. Performance indicators should allow us to answer two critical
questions: “Are we still relevant to the organization? And if
not, why not?” Until we can answer these questions objectively, we must
continue the search for valid and meaningful measures of performance.
References
Boekhorst, P. (1995). Measuring quality: The
IFLA guidelines for performance measurement in academic libraries. IFLA Journal, 21(4), 278-281.
Cameron, K. S. (1986). Effectiveness as paradox:
Consensus and conflict in conceptions of organizational effectiveness. Management
Science 32(5): 539-553. doi:
10.1287/mnsc.32.5.539
Chan, A. P. C., &
Chan, A. P. L. (2004). Key performance indicators for measuring construction success. Benchmarking: An International
Journal, 11(2), 203-221. doi:
10.1108/14635770410532624
Donabedian, A. (1966, 2005) Evaluating the quality of medical
care. Milbank Quarterly, 44:
166-203. Reprinted in Milbank Quarterly, 83(4), 691–729. doi: 10.1111/j.1468-0009.2005.00397.x
Geier, D. B. (2007). Prevent a disaster in your library: Advertise. Library Media
Connection, 25(4), 32-33.
Harrison,
J., Creaser, C., & Greenwood, H. (2011). Irish health libraries: New
directions: Report on the status of health librarianship & libraries in
Ireland (SHeLLI ). Retrieved 13 Oct. 2012 from http://hdl.handle.net/10147/205016
Hauser,
J. R., Katz, G. M., & International Center for
Research on the Management of Technology. (1998). Metrics: You are what you
measure! Working papers 172-98, Massachusetts Institute
of Technology (MIT), Sloan School of Management. Retrieved 13 Oct. 2012
from http://web.mit.edu/~hauser/www/Papers/Hauser-Katz%20Measure%2004-98.pdf
Health Act
2004 (Ireland). (2004). In Irish
Statute Book. Retrieved 13 Oct. 2012 from http://www.irishstatutebook.ie/pdf/2004/en.act.2004.0042.pdf
Health Information and Quality Authority (2010). Guidance on developing key performance indicators and minimum
data sets to monitor healthcare quality.
Dublin: HIQA. Retrieved 13 Oct. 2012 from http://www.hiqa.ie/system/files/HI_KPI_Guidelines.pdf
Health
Service Executive (2012). HSE West service plan 2012.
Ireland: HSE West. Retrieved 13 Oct. 2012
from http://www.hse.ie/eng/services/Publications/corporate/westserviceplan2012.pdf
Health
Service Executive (2011). HealthStat – metrics and targets. Retrieved 13 Oct. 2012 from
HSE website http://www.hse.ie/eng/Staff/Healthstat/metrics/
Health Service Executive Health Promotion Unit &
National Adult Literacy Agency (2010). Plain language
style guide for documents. Dublin: Health Service Executive.
Retrieved 13 Oct. 2012 from http://hdl.handle.net/10147/98048
Health
Service Executive & Royal College of Surgeons Ireland. (2010). Report of the national acute medicine programme. Dublin:
Health Service Executive. Retrieved 13 Oct. 2012 from http://www.hse.ie/eng/services/Publications/services/Hospitals/AMP.pdf
Holst,
R., Funk, J. C., Adams, H. S., Bandy, M., Boss, C. M., Hill, B., Joseph, C. B.,
& Lett, R. K. (2009). Vital pathways for hospital librarians: Present and
future roles. Journal of the Medical
Library Association, 97(4),
285–292. doi:
10.3163/1536-5050.97.4.013
Kaplan,
R. S., & Norton D. P. (1992). The balanced scorecard: Measures that drive performance. Harvard
Business Review, 69(1), 71–79.
Klein,
M. W., Malone, M. F., Bennis W. G., & Berkowitz,
N. H. (1961). Problems of measuring
patient care in the outpatient-department. Journal
of Health and Human Behavior, 2(2), 138–144.
Levis, M., Brady, M., & Helfert,
M. (2008). Information
quality issues highlighted by Deming’s fourteen points on quality management.
International
Conference on Business Innovation and Information Technology (ICBIIT), 24
January 2008, Dublin City University, Ireland. Retrieved 13 Oct. 2012 from http://www.tara.tcd.ie/bitstream/2262/40479/1/ICBIIC_V2.pdf
Loeb, J. M. (2004). The current
state of performance measurement in health care. International Journal for Quality in Health Care, 16(Suppl.1):
i5-i9.
Marshall, J. G. (1992).
The impact of the hospital library on clinical decision making: The Rochester
study. Bulletin of the Medical Library
Association, 80(2): 169-78. Retrieved 13 Oct. 2012 from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC225641/pdf/mlab00115-0079.pdf
Matthews, J. R. (2008). Scorecards for results: A guide for
developing a library balanced scorecard. Westport, CT: Libraries Unlimited.
Md Ishak, A. H., & Sahak, M. D. (2011). Discovering the right key performance indicators
in libraries: A review of literatures. Paper presented at the 1st PERPUN
International Conference and Workshop on Key Performance Indicators for
Libraries 2011, 17-19 October 2011, Universiti Teknologi Malaysia, Johor Bahru. Retrieved 13
Oct. 2012 from http://eprints.ptar.uitm.edu.my/4120/1/D1_S2_P3_330_400_AMIR_HUSSAIN__6.pdf
Olmsted, M. G., Murphy, J., McFarlane, E., & Hill, C. A. (2005). Evaluating methods
for increasing physician survey cooperation. Paper presented at the
60th Annual Conference of the American Association for Public Opinion Research
(AAPOR), Miami Beach, FL, May 2005. Retrieved 13 Oct. 2012 from http://www.rti.org/pubs/olmstedpresentation.pdf
Parmenter, D. (2010). Key performance indicators: Developing,
implementing, and using winning KPIs. New Jersey: Wiley.
Ritchie, A. (2010, March
29-April 1). Thriving not just surviving:
Resilience in a special library is dependent on knowing why you exist (not
simply what you do). Paper presented at ALIES 2010 Conference: “Resilience”
29 Mar-1 Apr 2010. Retrieved 13 Oct. 2012 from http://www.em.gov.au/Documents/Ann%20Ritchie%20-%20NT.PDF
Tukey, J. W.
(1962). The future of data analysis. Annals of Mathematical Statistics,
33(1), p. 1-67.
Wadsworth, T., Graves, B.,
Glass, S., Harrison, A.M., Donovan, C., & Proctor, A. (2009). Using business intelligence to improve performance. HFM
(Healthcare Financial Management), 63(10), 68-72.
Warner,
D. G. (2001). A new
classification for reference statistics. Reference & User
Services Quarterly, 41(1): 51-55.
Weightman, A. L., & Williamson, J. (2005). The value and impact of information provided through
library services for patient care: A systematic review. Health Information & Libraries Journal, 22(1): 4-25. doi: 10.1111/j.1471-1842.2005.00549.x.
WHO Regional Office for Europe’s Health Evidence
Network (HEN) (2003). How can hospital performance be measured and monitored? Copenhagen: WHO. Retrieved 13 Oct. 2012 from http://www.euro.who.int/__data/assets/pdf_file/0009/74718/E82975.pdf
![]() 2012 Dalton.
This is an Open Access article distributed under the terms of the Creative
Commons‐Attribution‐Noncommercial‐Share Alike
License 2.5 Canada (http://creativecommons.org/licenses/by-nc-sa/2.5/ca/),
which permits unrestricted use, distribution, and reproduction in any medium,
provided the original work is properly attributed, not used for commercial
purposes, and, if transformed, the resulting work is redistributed under the
same or similar license to this one.
2012 Dalton.
This is an Open Access article distributed under the terms of the Creative
Commons‐Attribution‐Noncommercial‐Share Alike
License 2.5 Canada (http://creativecommons.org/licenses/by-nc-sa/2.5/ca/),
which permits unrestricted use, distribution, and reproduction in any medium,
provided the original work is properly attributed, not used for commercial
purposes, and, if transformed, the resulting work is redistributed under the
same or similar license to this one.